Painful Sex & Physical Discomfort: A Complete Guide to Dyspareunia and Vaginismus
Sex should be pleasurable, but for millions of women, it feels like pressure, burning, or even trauma. Painful sex — whether caused by dyspareunia or vaginismus — is real, medical, and solvable. It’s time to break the silence, understand the science, and explore holistic paths to healing.
What Is Painful Sex?
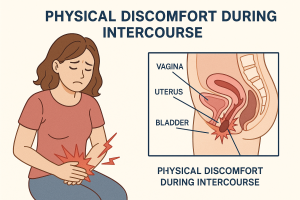
Painful sex, medically called dyspareunia, is defined as persistent genital or pelvic pain that occurs just before, during, or after vaginal penetration. It can be sharp, burning, stabbing, or feel like unbearable tightness. For some, it triggers emotional fear or full-body tension.
Two Main Clinical Diagnoses:
- Dyspareunia: Pain during or after vaginal penetration, caused by physical, hormonal, or neurological conditions.
- Vaginismus: Involuntary spasms of the pelvic floor muscles that prevent penetration. Often psychologically rooted.
Pain during sex is not just physical — it affects body image, emotional intimacy, and partner trust.
Key Symptoms (Often Overlapping)
- Sharp pain or tearing sensation upon entry
- Burning or stinging, especially near vaginal opening
- Cramping or pelvic muscle pain during or after sex
- Feeling of tightness or “hitting a wall”
- Panic, fear, or emotional shutdown when touched intimately
These symptoms are not a sign of failure. They are your body asking for care, not force.
Why It Matters
- Trust Breakdown: Pain undermines emotional safety and creates fear around intimacy.
- Emotional Trauma: For some women, each painful attempt reinforces trauma loops.
- Biological Disconnection: The brain learns to associate arousal with fear or threat.
- Silent Suffering: Most women never tell their partner. They search online late at night, isolated.
Research shows 75% of women who experience painful sex never receive proper diagnosis or treatment.
Common Causes
Physical Causes:
- Postpartum changes (episiotomy, scar tissue, hormonal shifts)
- Menopause or estrogen deficiency
- Endometriosis or pelvic inflammatory disease (PID)
- Infections (yeast, bacterial, UTI)
- Scar tissue from surgeries or trauma
- Vaginal dryness or thin tissue (atrophic vaginitis)
Psychological or Neuromuscular Causes:
- Previous sexual trauma or abuse
- Negative sexual conditioning or shame
- Chronic stress or anxiety
- Fear of pain / pain anticipation cycle
- Pelvic floor hypertonicity
Diagnosis often requires a trauma-informed pelvic exam and discussion of emotional triggers.
Behavior Patterns (What Clinicians See)
1. “There’s something wrong with my body.”
Women internalize the pain as failure or defect. Many try to “push through it” to satisfy their partner, which worsens both symptoms and self-esteem.
2. Silent Researcher
Women often search online in private, late at night, desperate for answers. They rarely speak to partners or doctors. Shame silences them.
3. Misunderstood by Partners
Partners may react with confusion, frustration, or withdrawal — further deepening emotional disconnection.
What Is Yoni Therapy?
Yoni therapy is a holistic, body-based healing practice that addresses trauma, tension, and numbness in the pelvic space. It combines physical, energetic, and emotional techniques to restore trust in the body.
How It Helps Painful Sex:
- Reconnects mind-body awareness to the pelvic region
- Gently releases stored trauma or tension in vaginal tissue
- Supports re-patterning of pain/fear responses
- Encourages healthy boundaries and safety before pleasure
- Increases vaginal lubrication and blood flow
- Normalizes loving, non-penetrative touch
Yoni therapy may involve:
- External pelvic massage
- Breathwork and guided body awareness
- Internal yoni de-armoring (with consent)
- Somatic dialoguing to rebuild trust
This is not sexual service — it is therapeutic, consensual, and trauma-informed care.
Recovery: What Works
1. Trauma-Informed Pelvic Therapy
Certified pelvic floor physical therapists can help identify internal imbalances and retrain the muscles through biofeedback, dilation, and manual therapy.
2. Psychological Support
Therapy with a sex-positive psychologist trained in trauma can help unwind shame, fear, or past abuse narratives.
3. Somatic Therapy and Yoni Massage
Helps regulate the nervous system, restore body trust, and safely explore boundaries. Best when paired with professional support.
4. Lubrication and Vaginal Estrogen (for menopause)
In postmenopausal women, topical estrogen and pH-balanced lubes can dramatically reduce atrophy-related pain.
5. Partner Education
Partners who understand the cause, don’t take it personally, and support healing — not penetration — accelerate recovery.
Myths to Break
| Myth | Truth |
|---|---|
| “Just relax” | Pain is not caused by tension alone. It’s physiological and emotional. |
| “It’s all in your head” | Psychological trauma shows up in real muscle patterns. |
| “Lube fixes everything” | Lube helps, but does not treat muscle spasms or trauma. |
| “You’ll grow out of it” | Without intervention, symptoms often worsen. |
| “Pain means no arousal” | Many women feel desire even while fearing penetration. |
Final Thoughts: Healing Is Possible
Painful sex is not rare. It is not shameful. And you are not broken. Whether your pain stems from birth trauma, hormonal shifts, surgery, or emotional injury — it can be addressed. But healing starts with listening to your body, not forcing it.
You are not alone. You deserve safety, pleasure, and intimacy that doesn’t hurt.
Start with curiosity. Seek the right support. And let your healing be led by compassion, not shame.

 Tags:
Tags: